Mental health issues are more common than many people realize. According to the National Alliance on Mental Illness (NAMI), nearly 1 in 5 American adults experience some form of mental illness every year. Despite how widespread these issues are, there remains a stigma around seeking help for mental health that prevents many people from getting the treatment they need. Knowing when it’s time to seek professional care can greatly benefit both your short-term ability to cope and long-term mental health and wellbeing.
Recognizing Signs That It’s Time for Help
Deciding when to seek help isn’t always straightforward. Many people dismiss serious symptoms or wait until they can no longer cope on their own. Learning to identify key signs that indicate it’s time to get support can make a major difference:
Changes in Daily Life and Relationships
* Difficulty carrying out responsibilities at work, school, or home
* Withdrawing from friends, family, and enjoyable hobbies or activities
* Significant deterioration of hygiene, appearance, or personal living spaces
* Fighting more with loved ones or loss of intimate relationships
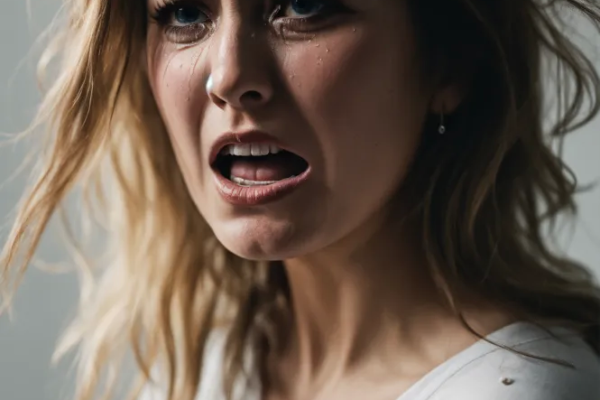
Worsening Mental Health Symptoms
* Dramatic shifts in sleep, appetite, energy level, concentration, or mood
* Inability to control worry, panic attacks, scary thoughts or flashbacks
* Growing severity or frequency of symptoms like depression, anxiety, anger etc.
* Onset of thoughts about death, dying or suicide
Failure of Self-Care Strategies
* Inability to alleviate symptoms through things like exercise, meditation, therapy workbooks, support groups etc.
* Prescribed medications become less effective over time
* Progressively relying on unhealthy coping mechanisms like substance abuse
Intuition and Input from Others
* A gut sense that things are getting worse and outside help is needed
* Comments from loved ones expressing concern over recent behavior changes
* Friends or family members suggest seeking professional treatment
Common Types of Mental Health Professionals
If you recognize the signs that it’s time to seek help, the next step is figuring out which type of mental health professional to turn to. Here are several common options:
Psychiatrists
Psychiatrists are medical doctors who specialize in diagnosing and treating mental illnesses. Unlike other mental health professionals, psychiatrists can prescribe medication. Seeing one can be a good option if you think you might benefit from psychiatric drugs.
Psychologists
Psychologists have an advanced degree focused on diagnosing and treating mental health conditions through methods like psychotherapy and counseling. There are many types, including clinical, developmental, forensic and social psychologists.
Therapists and Counselors
There are various types of therapists and counselors trained to help people through issues like family conflicts, grief, low self-esteem, stress and emotional difficulties. Four of the most common are family and marriage, mental health, school and substance abuse counselors.
Social Workers
Social workers support people dealing with issues like poverty, neglect, addiction, disability, trauma and lack of healthcare or community resources. Their goal is to enhance overall wellbeing by connecting clients with beneficial services and guidance.
Questions a Mental Health Professional May Ask During Your First Visit
That first appointment with a psychiatrist, therapist or other mental health pro can seem intimidating. Preparing for some of the questions they’re likely to ask can help ease uncertainty over what to expect:
Background Questions
* What prompted you to schedule this appointment today?
* When did you first start noticing an issue?
* Have you received any prior diagnoses or treatment?
* Does anyone in your family have similar mental health conditions?
Lifestyle and Health Questions
* How much/well are you sleeping and eating compared to your normal?
* Do you exercise, smoke, drink alcohol or use any substances?
* Are you experiencing any unexplained physical symptoms?
* What medications or supplements do you currently take?
Support System Questions
* How fulfilled do you feel in your relationships with friends and family?
* Do you have someone you can call with emotional needs at any time?
* Are there any major stressors related to finances, work, relationships etc.?
Symptom Questions
* What feelings or challenges are interfering with your day-to-day life?
* Can you recognize any thought or behavior patterns contributing to symptoms?
* Have you ever thought about harming or attempting to harm yourself?
Remember, mental health pros aren’t there to judge you. Don’t feel embarrassed or afraid to be totally open so you get the care you truly need.
Factors That May Influence Getting Help for Mental Health Issues
There are many potential barriers that keep people suffering from mental illness from seeking help from a professional. Recognizing how any of the following apply to you can help you push past them:
Stigma and Shame
Despite society making great strides in destigmatizing mental illness, shame surrounding diagnoses and symptoms still deters many from admitting they need support. Challenging inner criticism and negative self-talk is key.
Lack of Insight
Some conditions like schizophrenia spectrum disorders impair insight and make it hard to evaluate strange behavior as problematic. Getting perspective from a loved one can provide clarity.
Fear and Distrust
Bad prior experiences or anxiety over what treatment entails leads some to avoid help. Starting with an evaluation versus long-term commitment can help overcome this hurdle.
Financial Barriers
Between intake exams, therapy fees and prescription costs, getting mental healthcare can be prohibitively expensive, especially for severe issues requiring extended treatment. Check if insurance, local nonprofits or state-funded programs offer affordable access.
Available Provider Shortages
Even those fully committed to treatment often face long waitlists, particularly in rural areas and low-income communities with few practitioners. Expanding your search radius and interim group support can help bridge the gap.
Overcoming mental health stigma, fear over the unknown, doubt you deserve help and obstacles to access takes courage and resilience. But moving past these roadblocks can put you on the path toward reclaiming joy and purpose.
Questions to Consider Before Your First Therapy Session
Preparing questions ahead of time can help guide your initial mental health evaluation toward providing maximum insight for effective treatment planning. Some important ones to consider asking include:
* What are your credentials, areas of specialty and therapeutic approach?
* What might an average treatment plan look like based on my symptoms?
* How will we measure progress as I undergo treatment over time?
* Do you incorporate other self-care like nutrition, physical activity, mindfulness?
* Will there be ‘homework’ for me or participation between sessions?
* Are long-term medications likely to be part of my treatment?
* What out-of-session resources do you recommend if extra support is ever needed?
* What type of confidentiality and transparency practices do you follow?
* Do you take notes, keep recordings or monitor emails/calls in any capacity?
* How much do services cost, what payment options do you accept and is contingency paperwork required to move forward today?
Having a dialog about diagnosis methodology, therapy techniques, visibility into progress markers, involvement expectations, additional support structures, privacy protection standards and potential constraints around timelines or cost provides the clarity needed to determine if a provider relationship feels like an optimal fit.
Setting Realistic Expectations for the Process
Just as no two people’s mental health challenges manifest exactly the same way, no two paths to wellbeing look identical either. Setting realistic expectations around the process prevents losing hope from comparing your timeline or outcomes to others’ experiences. Remember that:
* Finding an effective professional match often takes meeting multiple providers
* Progress tends to be gradual, with ups and downs vs linear improvement
* Periodic med adjustments are common when psychiatric drugs are involved
* Breakthrough moments rarely happen quickly after just a session or two
* Long term consistency is key, sporadic or crisis-only support less effective
* Recovering from complex or chronic issues can take many months to years
* Ongoing self-care routines outside clinical visits optimize outcomes
Patience, personal agency and trust in the methods agreed upon with your counselor or doctor – while pivoting approaches if reasonable timeframes show minimal gains – lays the foundation for mental health growth possible over time.
Warning Signs That a Crisis May Be Developing
While finding a therapist and developing a long-term treatment plan is ideal for many facing mental health struggles, sometimes issues can escalate faster, requiring more immediate support. Emergency warning signs to take seriously right away include:
Losing Touch With Reality
* Hallucinations like hearing voices or seeing things others can’t detect
* Expressing beliefs drastically out of sync with actual circumstances
* Conveying irrational thoughts or behaviors those around you don’t understand
Risk of Harm
* Threatening to injure or kill someone else
* Indicating plans to seriously harm or attempt suicide yourself
Intensifying Mental Distress
* Panic, rage, paranoia, despair or emotional pain growing unmanageable
* Inability to sleep, function or care for personal needs for multiple days
Withdrawal and Isolation
* Severe detachment from loved ones, social settings or previously enjoyed activities
* Limited communication through dropped calls, texts and skipped visits over a concerning timeframe
If you or someone you know exhibits these types of patterns, seeking help right away can be pivotal in preventing further crisis escalation. Call emergency services, visit an urgent psychiatric clinic or emergency room, request a welfare check by law enforcement or leverage crisis intervention resources in your area at the first signs of instability requiring immediate support.
Options for Crisis Lines and Hotlines
When facing an emerging mental health emergency, crisis lines and hotlines connected to trained counselors and local mental health resources can provide interim guidance on the best path forward while more comprehensive treatment is arranged. If you or a loved one feels unable to cope or unsafe during a crisis moment, calling one of the following options is strongly advised:
* **National Suicide Prevention Lifeline** – Call or text 988 to speak with a crisis counselor at any hour of the day or night, any day of the week. Specialists are also available via online chat at suicidepreventionlifeline.org.
* **SAMHSA Treatment Referral Hotline** – Call 1-800-662-HELP (4357) for free confidential support and treatment recommendations 24/7. Assistance available for substance abuse, mental health needs and general crisis intervention.
* **Crisis Text Line** – Text HOME to 741741 in the U.S. or 686868 in Canada to chat with a trained crisis counselor.
* **The Trevor Project** – Call 1-866-488-7386, text START to 678678 or chat online at TheTrevorProject.org/Get-Help-Now. Specialized support for LGBTQ youth in crisis.
* **Veterans Crisis Line** – Connect with the U.S. Department of Veterans Affairs by calling, texting or chatting online when struggling with mental health distress as a veteran or military member.
* **Local Hospital or Police** – Calling 911, showing up to an ER or requesting an in-person law enforcement welfare check are additional options if other crisis lines feel unresponsive or risks seem too high based on visible warning signs present.
Seeking help through hotlines is often the critical first step toward de-escalating a mental health crisis until additional treatment can be secured following emergency triage. Don’t hesitate to leverage these free, easily accessible resources.
Overcoming Stigma Around Mental Healthcare
Despite greater awareness and acceptance of mental illness over recent years, significant stigma persists around seeking treatment that prevents many from getting the help they deserve. Challenging misconceptions with facts and having compassion for struggles faced can help dismantle prejudices.
The reality is mental health conditions are extremely common. In fact:
* 50% will have a diagnosable issue in their lifetime
* 20% experience symptoms yearly
* 4% live with a seriously disabling condition
* 9 out of 10 people with substance abuse disorders have co-occurring mental illness
Yet outdated beliefs painting those facing anxiety, depression, OCD, PTSD, bipolar disorder or schizophrenia as unstable, immoral, irrational or deserving blame over symptoms leads to fear about admitting needs due to:
* Perceived weakness or failure for being unable to independently “get over it”
* Fear peers and employers will judge struggles as deficiencies or character flaws
* Minimization that symptoms constitute “real” health issues requiring compassionate medical care like physical injuries or diseases
But the brain is simply another organ vulnerable to episodic or chronic illness just like the heart, lungs or liver. Seeking mental healthcare demonstrates self-awareness, courage and commitment to wellness – it should be destigmatized and applauded the same as pursuing treatment for diabetes, cancer or gluten intolerance.
Only by speaking out, showing compassion toward those affected and advocating for health equality can we encourage others to access vital care without shame or secrecy. The opportunity to live a meaningful, purposeful life lies on the other side of asking for help when needed.
Exploring Available Mental Health Resources
Navigating countless therapists, psychiatrists, community mental health centers, crisis lines and support groups often proves confusing for those first seeking help – leading many to ask “Where do I even start?”. Several options to research local mental health resources exist, including:
* **Online Database Searches** – Platforms like Psychology Today, GoodTherapy and Zencare allow filtering by cost, location, specialty, insurance and availability.
* **Primary Care Referrals** – Discussing symptoms with your general practitioner allows accessing referrals informed by full medical history.
* **Local Advocacy Centers** – Organizations like county mental health associations and NAMI chapters help connect people to care.
* **Hospital Systems** – Larger regional medical centers often have databases by diagnosis/demographics and assist with appt scheduling.
* **County Health Departments** – Government sponsored clinics provide needs assessments and care navigation, often on an income based sliding-scale.
* **Support Group Networks** – Peer communities for specific conditions act as information exchange hubs.
* **Educational Institutions** – Most colleges/universities offer free counseling to students through designated offices.
Casting a wide net through exhaustive personal research, medical referrals and local service directories allows compiling a list of viable options matching treatment preferences, health needs and accessibility. Don’t hesitate to enlist social workers, school/hospital case managers and nonprofit volunteers to further assist connecting the right care.
Questions to Consider if Symptoms Persist Without Improvement
Failing to experience any relief from mental health issues after months of proactive treatment can leave you feeling hopeless and frustrated. Before resigning yourself to ongoing struggles or abandoning care, first take time to reflect honestly on important diagnostics like:
Am I fully committing to the process?
* Attending every therapy and psychiatry session possible
* Taking all medications reliably at directed dosages and intervals
* Practicing skills and completing assignments outside appointments
* Engaging social, community and self-care support outlets
Does my treatment plan align to contributing factors?
* Were social, medical, genetic, trauma and personality drivers thoroughly assessed?
* Are multiple complementary modalities like talk therapy, group counseling and medications leveraged in a coordinated way?
Do my providers specialize in my areas of need?
* Seeking a highly targeted specialist vs a generalist practitioner
* Working with a team attacking factors from different angles
Could an underlying condition be the true culprit?
* Heavy substance abuse masking or aggravating disease progression
* Autism Spectrum or personality disorders complicating communication
* Thyroid dysfunction, hormonal imbalance, Lyme disease or nutrient deficiency triggering chemical depression
If after reexamining these considerations you remain concerned over limited gains, don’t simply tolerate ongoing distress – advocate to adjust approaches until discovering the exact customized protocol meeting your needs. With close collaboration between client and caregiver, better outcomes emerge.
Creating a Mental Health Crisis Intervention Plan
Experiencing periodic setbacks while on the road to recovery from mental illness is perfectly normal. But uncontrolled flare ups of symptoms can quickly snowball into full blown psychiatric emergencies. Creating a crisis contingency plan helps de-escalate detrimental tailspins through automatic built-in supports.
Essential elements to define include:
Recognizing Early Warning Signs
* First indications of thoughts/behaviors signaling upcoming loss of function
Internal Coping Strategies
* Go-to anxiety reduction, emotion regulation or distraction skills to deploy independently
Support Team Notification Protocols
* Who to contact and how among friends, family members or providers if extra help becomes necessary
Professional Crisis Service Options
* Steps to access therapists, psychiatrists, crisis lines/hotlines or inpatient stabilization
Medication Adjustment Guidelines
* When and how to leverage PRNs like benzodiazepines or temporarily increase dosages
Safeguarding Measures
* Voluntarily restricting access to firearms, car keys, bank accounts if suicidal ideation emerges
Medical Rights Delegation
* Signed releases enabling loved ones to interface with institutions on your behalf
By recognizing individual tipping points through granular tracking of mood variability then lining up tailored contingencies spanning natural supports up through emergency services, you remain empowered to self-advocate needs during vulnerable moments. Don’t wait for desperation before planning tools to endure the storm.
Finding Hope through Shared Mental Health Experiences
Battling anxiety, depression, PTSD and other psychiatric disorders often leaves you feeling desperately alone. Many assume no one else suffers similar struggles privately endured. But shifting perspective to recognize just how universal mental health challenges reach across all cultures, ages and walks of life breeds solidarity.
Listen as the stories below mirror pieces of your own:
**_Sarah, 42 – Stay at Home Mom_**
Between endless house chaos, pressure to be “on” 24/7 for needy kids and keeping a lackluster marriage afloat – I crawled under rising tides of resentment and loneliness. Masking cracks to portray Pinterest perfection left me crumbling inside.
**_Michael, 28 – Grad Student_**
Struggling under crushing student debt while fighting diagnosed OCD, everyone praised me as high functioning. But paralyzing anxiety constantly triggered avoidance spirals. I couldn’t risk failure yet felt directionless about my future.
**_Fatima,




